Applying a Rights-based Approach to Fulfill Maternal Health Obligations
Meaningful and equitable progress on reducing maternal mortality and meeting Millennium Development Goal 5 calls for the adoption of a human rights-based approach which emphasizes ‘accountability.’ This article focuses specifically on how to promote accountability for fulfilling the right to maternal health if we seek to transform the discourse of rights into practical health policy and programming tools that can affect development practice–and in turn to transform health systems to better meet women’s maternal health needs.
After briefly discussing the concept and purpose of accountability in the context of fulfilling women’s rights to maternal health, the article then sets out a circle of accountability at the national level that includes: development and implementation of a national plan of action; budgetary analysis; monitoring and evaluation of programs based on appropriate indicators; and mechanisms for redress, as well as facility-level initiatives. In the final section the article addresses donor accountability.
The great majority of women who die as a result of pregnancy-related complications have lived lives marked by poverty, deprivation and discrimination. From the moment of their births, these girls and women often face a funnel of narrowing choices whereby they are unable to exercise meaningful agency with respect to what they will do with their lives, how much they will be educated, with whom they will partner, when they will have sex, whether they will use contraception, and finally what care they will get when they are pregnant or delivering, even when their lives hang in the balance. Adopting a rights-based approach to women’s health demands opening spaces for women to exercise choices and subverting the social – and power –relations that deny them their full humanity (YAMIN, 2008) . With respect to maternal morbidity and mortality (MMM)2 in particular, a rights-based approach calls for challenging the structural discrimination women face in health systems, as well as in other spheres of public and private life.
As it has become increasingly clear that meaningful and equitable progress on Millennium Development Goal (MDG) 5, which relates to maternal health, will require more than adding funding to existing technocratic approaches, there has been increasing attention to rights-based approaches to maternal mortality. In June 2009, the UN Human Rights Council (HRC) issued a historic resolution that explicitly recognized preventable maternal mortality as a human rights issue, and signaled the important role that could be played by treaty-monitoring committees and special procedures (UNITED NATIONS, 2009a) . The HRC is now in a position to adopt a meaningful follow-on resolution based upon the recommendations of a study by the UN Office of the High Commissioner on Human Rights (OHCHR), which further elaborates the connections between human rights and MMM (UNITED NATIONS, 2010a) .
Initiatives calling for rights-based approaches to MMM all emphasize accountability, which has been lacking in the MDGs process (UNITED NATIONS, 2010b, para. 116) . For example, the OHCHR publication relating to the MDGs process overall, Claiming the Millennium Development Goals: A Human Rights Approach , explains “the raison d’etre of the rights-based approach is accountability” (LANGFORD, 2008, p. 15) . The UN Special Rapporteur on the right to health underscored the importance of accountability in human rights approaches to maternal mortality (UNITED NATIONS, 2006a). Further, non-governmental organizations (NGOs) also explicitly focus on the centrality of developing effective accountability (IIMMHR, 2010, p. 3; HUMAN RIGHTS WATCH, 2009, 2010; CRR, 2009).
Accountability in a human rights-approach to maternal health relates to obligations to “respect, protect and fulfill” a wide array of civil and political rights, as well as economic and social rights, and goes far beyond the health sector3 (UNITED NATIONS, 2000). Not only is maternal mortality fundamentally linked to women’s social and economic status in society, but gender inequality and violations of women’s sexual and reproductive rights constitute grave injustices even when they are not directly related to women’s deaths or morbidity (ICPD, 1994; UNITED NATIONS, 1999). A comprehensive rights-based accountability framework with respect to MMM requires the explication of these multiple obligations relating to all relevant rights.
However, this article focuses on the specific issue of how to promote accountability for fulfilling –for taking proactive steps to progressively realize–women’s rights to maternal health if we seek to transform the discourse of rights into practical health policy and programming tools that can affect development practice–and in turn to transform health systems to better meet women’s needs. Revisiting how we understand ‘accountability’ in the context of fulfilling rights to maternal health is especially urgent given the opportunities presented by the upcoming MDG 2010 Review, the deliberations underway at the HRC, and incipient efforts to explore a post-2015 development agenda that includes a robust human rights dimension.
I begin by briefly setting out the concept and purpose of accountability in the context of fulfilling women’s rights to health and suggesting that pursuing effective accountability in this arena requires moving beyond the traditional human rights model of punishing individual perpetrators, to focus on institutional and systemic factors. The article then sets out a circle of accountability at the national level that includes: development and implementation of a national plan of action; budgetary analysis; monitoring and evaluation of programs based on appropriate indicators; and mechanisms for redress. I also discuss measures that can be taken at the facility level to increase “constructive accountability.” Throughout the article I argue that accountability is closely linked to meaningful popular participation. In the final section I specify aspects of accountability for “international assistance and cooperation,” which require donors to refrain from certain policies as well as to contribute greater resources.
In general, the concept of accountability refers to holding actors responsible for their actions in light of standards of behavior and performance. In a human rights framework, those standards are derived from both so-called “hard” and “soft” law sources, including inter alia binding international treaty norms and statements from quasi-judicial international bodies relating to the adjudication of pertinent cases, as well as authoritative interpretations of relevant norms by treaty bodies, statements by UN Special Rapporteur on the Right to the Highest Attainable Standard of Health, and international conference declarations and programmes of action. They are also informed by domestic constitutional frameworks, legislation and regulations. However, fostering accountability in practice requires more than setting out norms in the abstract and establishing enforcement mechanisms. It requires a dynamic process of clarifying legal standards for actors at various levels, from health service providers to policy-makers, and engaging with those actors with respect to the implications for their roles and responsibilities ( UNITED NATIONS, 2006b; GEORGE et al., 2010) .
In a human rights framework, accountability combines elements of responsiveness, answerability and redress. Moreover, accountability is necessarily relational— i.e ., there can be no human rights accountability without specifying ‘to whom?’—and therefore it is closely linked to the effective participation of people affected by health policies and programs (POTTS, 2008, p. 7) . In the context of reforming health systems to meet maternal health needs, accountability entails financial, administrative, regulatory, political and institutional dimensions, as well as legal recourse (UNITED NATIONS, 2006b) . As Amnesty International’s 2010 Report states, accountability “allows us to look ahead” as well as back (AMNESTY INTERNATIONAL, 2010, p. 10) . An effective framework of accountability serves as the basis for promoting systemic and institutional changes that create conditions under which women can enjoy their rights to maternal health, and not just for punishing identified lapses in performance.
Indeed, the traditional model of human rights advocacy, which seeks to identify a violation, a violator and a remedy is poorly suited to advancing accountability for improvement of maternal health. This is true for both practical and conceptual reasons. In practice, many health systems in which patients face abuses are extremely punitive with respect to front-line healthcare workers as well. For example, it is routine in many countries for health professionals who are associated with a maternal death to be summarily dismissed, without any procedure to discern whether they were in fact responsible for the death. These often unwritten policies are ostensibly intended to promote “accountability” and quality care in obstetric cases; they have the opposite effect. They create perverse incentives for health professionals to avoid dealing with obstetric emergencies, both as individuals and as institutions.
This does not mean a license for impunity. As Lynn Freedman (2003, p. 112) writes, “Of course, individual punishment (and knowledge that professional standards will be enforced) has an appropriate place in a constructive accountability system. The important point here is that individual sanctioning has not been used to scapegoat a doctor, pacify the public, and cover up wider, deeper problems”. When an individual provider could have done nothing to save a woman placing blame on him or her not only distorts incentives; it also diverts attention from the systemic problems that resulted in the woman’s death. For example, the health center may lack the necessary supplies or drugs, or transportation. As Leslie London (2008, p. 72) argues, “frontline health workers are frequently unable to provide adequate access to care because of systemic factors outside their control and because of management systems that disempower them from acting independently and effectively”. Focusing on individual health practitioners’ conduct divorced from context in such a situation, as London (2008, p. 73) writes, “frequently makes little headway and gives a human rights approach a bad name”.
“Maternal death audits” and “reviews”, whereby individual deaths of women are investigated with the aim of promoting reflection on institutional and systemic failures as well as individual failures, have been advanced by some as a means to promote “human rights based accountability” (HUNT, 2008; WHO, 2004) . Such reviews are done in myriad ways and therefore it is difficult to generalize. However, in general, as Human Rights Watch notes in its report on India, these reviews have a place in a broader accountability system, provided that they meet the following criteria: 1. they are conducted under strict confidentiality; 2. they provide for due process; and 3. the scope of the investigation extends beyond the facility (HUMAN RIGHTS WATCH, 2009) . When these conditions cannot be guaranteed there is a serious risk of backlash against human rights-based approaches by those health workers we most need as allies. Additionally—and critically—these reviews should be used to complement, rather than substitute for, the continuous use of process indicators that evaluate how the health system is functioning, e.g., to measure the use and availability of emergency obstetric care.
The model of identifying a violation, a violator and a remedy is conceptually inadequate as well. That is, it implicitly assumes that there is an equilibrium that is broken by the violation; an investigation can then be launched to determine culpability and provide redress to return the situation to equilibrium. This paradigm was developed to address violations of civil rights, such as abuses in police custody, where human rights advocates assumed (often incorrectly) that exposing and denouncing abuses could lead to punishment of perpetrators and deterrence of future harms. If this is often an invalid assumption with regard to civil rights abuses, it can be counterproductive with respect to fostering accountability with respect to fulfilling the right to maternal health.
In situations of high maternal mortality we are confronting dysfunctional health systems where deaths may be attributable neither to negligence nor to lack of oversight at the facility level, but to the lack of available blood, supplies, transport, communications and the like –which all call for systemic changes. Thus, grievance redressal mechanisms that do not go beyond the facility-level are likely to be ineffective, and in turn to foster even more disillusionment with unresponsive and poorly functioning health systems. True deterrence– which as Amnesty International’s 2010 Report notes is a principal goal of accountability (AMNESTY INTERNATIONAL, 2010) – requires transforming the underlying, untenable situation that gives rise to widespread MMM, not restoring a prior equilibrium. The rest of this article discusses what concrete ways in which to promote such transformation.
A comprehensive accountability framework for fulfilling the right to maternal health at the national level shapes the initial design of policies and programs to address maternal mortality, their implementation and evaluation, and the remedies provided in the event of violations. In this section, I draw out important elements of accountability that are promoted at each of these stages. Although I focus on actions to be taken at the national level, I suggest the adoption of simple steps at the facility level that empower both frontline health workers and community members to identify obstacles to and solutions for improving maternal health services as a means of promoting “constructive accountability.”
Although the right to health is subject to progressive realization and cannot be realized from one day to the next, States parties to relevant treaties undertake some immediate obligations, including the development of a national strategy and plan of action in respect of their public health goals (UNITED NATIONS, 2000, para. 43) . The UN Committee on Economic, Social and Cultural Rights (ESC Rights Committee) establishes the creation of a national public health strategy and plan of action, which is evidence-based and sets out deliberate targets, as one of a set of basic or core obligations that all states undertake as parties to the ICESCR ( UNITED NATIONS, 2000, para. 43) . Addressing maternal and reproductive health is an obligation of comparable priority and there is no country in the world where a national plan of action should not include attention to maternal health (UNITED NATIONS, 2000, para. 44) .
All such plans of action should be based upon a robust situational analysis regarding sexual, reproductive and maternal health in the country, as well as the best evidence of what interventions are required to address maternal morbidity and mortality (UNITED NATIONS, 2000, para. 43f) . The four pillars of reducing maternal mortality are now well-understood: skilled birth attendance, access to emergency obstetric care (EmOC), and a functioning referral network, together with family planning ( FREEDMAN et al., 2007) . Therefore, every national plan of action on maternal health must prioritize these four pillars in the context of strengthening the overall health system, as the “appropriate” measures to be adopting pursuant to international law, although legislative and programming measures will vary contextually based upon the situational analysis (UNITED NATIONS, 1966, art. 2; UNITED NATIONS, 2000; YAMIN; MAINE, 1999) . In keeping with international law, a national plan of action should also include a broad range of services related to sexual and reproductive health, which are aimed at enabling women to exercise agency with respect to their bodies and, in turn, their lives (ICPD, 1994, para. 7.2; UNITED NATIONS, 2000, para. 20-21; UNITED NATIONS, 1999) .
Under international law, the process of devising a national plan must be transparent and participatory, and its implementation must be subject to periodic evaluation, which is also public (UNITED NATIONS, 2000, para. 43f) . If maternal health is a matter of rights, the women who use health services are not objects of governmental charity or targets of a development policy designed elsewhere; they and their families are agents who have a role to play in the definition of programs and policies that structure the possibilities for their well-being. Therefore, participation cannot be hollow consultation; it must be linked to the policy decisions taken by a government (often in conjunction with a donor or multilateral institution). For example, the public is entitled not only to know whether health facilities are being required to provide for traditional birthing positions and other culturally appropriate care; civil society should be entitled to influence the definition of what constitutes culturally appropriate care.
Requiring policy decisions that affect people’s rights, including women’s rights to maternal health, to be justified and subjecting those justifications to public scrutiny is fundamental to accountability, and goes well beyond curbing patently arbitrary policies. There will always be questions that arise in the interpretation of a situational analysis or design of a national plan that are not technical in nature, but reflect profound value judgments. For example, although human rights requires non-discrimination and General Comment 14 calls for the national plan of action to give “particular attention to the vulnerable and marginalized,” (UNITED NATIONS, 2000; para 43f) there is no single answer to exactly how much priority should be placed on remote and under-served areas in comparison with impoverished and heavily populated peri-urban areas. In conventional, utilitarian public health or development programming, such decisions might be made based upon cost-utility calculations by groups of experts. However, in a human rights paradigm, such planning and budgeting must be subject to meaningful public deliberation.
The Rawlsian ethicist, Norman Daniels, proposes “accountability for reasonableness,” to ensure the justness of processes to set priorities in health (DANIELS, 2008) . To meet the standards of accountability for reasonableness, which is broadly consistent with human rights concerns, the process of devising a plan of action and setting priorities must be 1.subject to public justification; 2. reasonably related to the end of reducing maternal mortality and promoting maternal health; 3. enforceable; and 4. afford some form of appeal in certain circumstances, such as the evident neglect of a minority population (DANIELS, 2008; GRUSKIN; DANIELS, 2008) .
Plans of action can be suffused with rights-based principles but progress toward fulfilling the right to maternal health requires expenditure. Budgets often offer the best evidence of whether governments are actually making maternal health a priority (KGAMPHE; MAHONY, 2004) . Therefore, demanding transparency and accountability in budgets is a key to transforming health systems to meet women’s needs.
An innovative example of international advocacy around budgetary accountability is the “6 Question Campaign” whereby through the International Budget Partnership civil society organizations in 85 countries are assessing their governments’ commitment to MDG 5 among other issues. Two out of the six questions relate to maternal health, and specifically to expenditures for uterotonics and magnesium sulphate and the training of skilled midwives (INTERNATIONAL BUDGET PARTNERSHIP, 2010) . The results of the campaign are to be released just before the MDGs summit in September 2010, and in all likelihood will reveal as much about whether governments are willing to and capable of providing this information as how much money is being spent.
At times the budgetary issue is whether a state is devoting the “maximum extent of its available resources” to the right to health and to efforts to address maternal mortality in particular, in accordance with international human rights obligations. In The Missing Link: Applied budget work as a tool to hold governments accountable for Maternal Mortality Commitments , the International Initiative on Maternal Mortality and Human Rights (IIMMHR) draws on examples from Mexico, Tanzania and India to “underscore that the lack of real progress in reducing maternal mortality is unquestionably linked to the failure of governments to make maternal health a budgetary priority” (IIMMHR, 2010, p. 7) .
However, it is sometimes the case that substantial resources exist and may even be going into the health sector, but results are poor due to a wide ranging series of factors. These factors include: lack of capacity to absorb resources, ineffective investment of funds, weak financial management, poor procurement practices, limited oversight, and poor district level management in decentralized health care systems (INTERNATIONAL BUDGET PARTNERSHIP, 2001; KEITH-BROWN, 2005) . It is essential to go beyond the design of budgets to pinpoint accountability gaps in terms of allocation and implementation, in order to design targeted strategies, whether for corruption or for ineffective investment.
Among the most valuable information that budgetary allocation reveals from a human rights perspective relates to, “understanding who among the population is prioritized” which, in turn, “allows us to demonstrate whether the government is fulfilling its obligation of non-discrimination” (IIMMHR, 2010, p. 7) . For example, a 2007 report I wrote for Physicians for Human Rights, Deadly Delays: Maternal Mortality in Peru , showed that the government of Peru was misallocating federal health spending toward departments with fewer unmet basic needs. Thus, Huancavelica, a department with over 90% of the population with unmet basic needs, was receiving a fraction of the federal health spending per capita that other, largely urbanized coastal and wealthier departments were receiving.
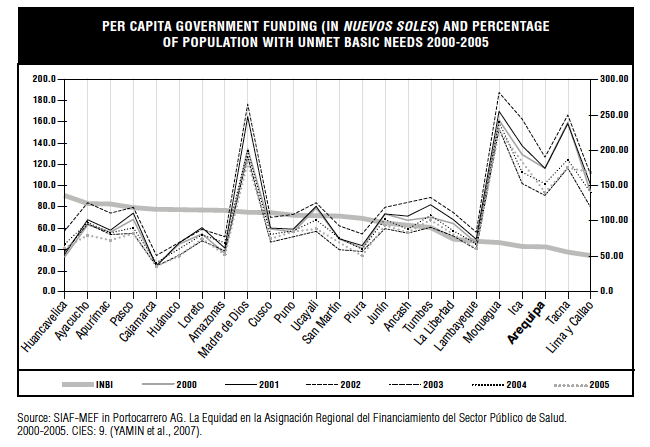
Moreover, the departments below the black line—that is, lower federal health spending per capita in comparison with unmet basic needs—had generally higher proportions of indigenous population than those departments above the black line.
In turn, the Deadly Delays report showed that, predictably, fewer resources resulted in fewer of the interventions necessary to save women’s lives. Huancavelica had a very low proportion of births attended by skilled personnel (21%), in comparison with other departments that received more health spending (YAMIN et al., 2007) . Peru’s own progress report on the MDGs at the time highlighted the unequal achievement of progress on MDG 5 (UNITED NATIONS, 2004a, p. 62) . Using a human rights framework that included budgetary analysis, however, enabled a recasting of those persistent disparities as substantive discrimination resulting from a misallocation of resources—discrimination which was entitled to redress (YAMIN et al., 2007) .
In a 2009 report on maternal health and other economic and social rights in Guatemala, the Center for Economic and Social Rights (CESR) also found misallocations of resources that correlated to ethnic lines and resulted in de facto discrimination. The CESR report went a step further by exposing the connections between Guatemala’s regressive and inadequate tax policies and its poor record on social spending, including on maternal health (CESR, 2009) .
Requiring governments to publicly justify their budgetary allocations as well as the policies that lead to insufficient available resources to spend on social policies, including maternal health, constitutes an important step in fostering systemic accountability. So does providing the public with the tools and information necessary to assess whether expenditures have been effective.
In order to open budgets, the promulgation of freedom of information laws is crucial. However, generating a culture of participation, accountability and transparency at all levels of government is necessary to make budgets more responsive to people’s, and in particular women’s, needs. In order to assure such a culture, capacity- building for civil society organizations in budget monitoring is essential. Moreover, donor states should be held to the commitments they have made in keeping with the Paris Principles and the Accra Agenda for Action to ensure transparency with respect to the way monies they provide or facilitate are spent, and similar requirements should be made of private donors ( OECD , 2008) .
Holding governments accountable for fulfilling the right to maternal health under international legal obligations requires monitoring “progressive realization.” Human rights advocacy groups are expert at assessing the adequacy of policy measures States are taking, as well as determining when they are adopting legislation or policies that indicate retrogression, such as restrictions on contraception availability or draconian abortion bans (AMNESTY INTERNATIONAL, Nicaragua, 2009a) . It is critical to identify such laws and policies, which constitute social determinants of MMM.
However, for both governments and advocacy groups, evaluating whether a state is making adequate progress on improving maternal health requires applying appropriate quantitative indicators. For example, as we are concerned with disparities as much as aggregate progress from a human rights perspective, it would be helpful to have disaggregated maternal mortality ratios (MMRs)—the indicator for whether states will achieve MDG 5(a). However, MMRs alone are inadequate as they rely upon data that is generally difficult to collect and interpret, for both statistical and practical reasons (MAINE, 1999) . Thus, for example, estimates of Sierra Leone’s MMR range from a low of 857 per 100,000 live births in the government’s latest Demographic and Health Survey (DHS) in 2009 to a high of 2,100 per 100,000 ( Sierra Leone, 2009; AMNESTY INTERNATIONAL, Sierra Leone, 2009b) . The truth is that we do not know what Sierra Leone’s actual MMR is, or what it will be in 2015, let alone actual regional disparities within the country. Moreover, MMRs alone do not tell us what the priorities are in terms of addressing MMM.
Therefore, in order for governments to measure their own progress– as well as for advocacy groups to hold them accountable for progressive realization–we need process indicators that: (1) can be measured continuously, so as to permit an assessment of the performance of a given administration; (2) are objective, and comparable across time and countries and/or sub-regions of countries; and (3) relate to the programmatic interventions that we know to be linked to reducing maternal deaths.
For example, data on met need for contraception and skilled birth attendance are critical, as are indicators such as access to anti-retroviral medications, especially in regions where there is a deadly synergy between the HIV epidemic and MMM (HOGAN et al., 2010) All of these indicators should be disaggregated by income quintile, race/ethnicity and region.
Indicators that measure the availability, distribution and use of emergency obstetric care (EmOC indicators) are also not only crucial, but can be being directly linked to requirements under international law that governments make the appropriate care available, accessible, acceptable and of adequate quality (the so-called AAAQ framework) (UNITED NATIONS, 2000, para. 12) . A 2009 (WHO et al., 2009) handbook sets out these updated EmOC indicators, which were devised by the WHO, Unicef, and UNFPA, in conjunction with the Averting Maternal Death and Disability program at Columbia University (AMDD). Importantly, the EmOC indicators can be monitored at both the district and the national level, as monitoring at a level “where there is power to effectuate change” is the key to transforming health systems (FREEDMAN et al., 2005)
Further, in the face of multi-factorial causes underpinning high maternal mortality, the EmOC indicators can prove extremely useful to governments in setting priorities and, insofar as these are made publicly available, to advocates in holding governments accountable for adopting the appropriate priorities. For example, the AMDD Handbook contains an exercise that presents three scenarios. In Scenario 1, there are three functioning EmOC facilities for nearly 1 million people rather than the 10 that is set as a minimum acceptable level, and they are mostly in urban areas. Although the other indicators are poor as well, the lack of availability of care stands out. When made publicly available, as it should be, this information allows advocates, as well as government program planners, to give first priority to accountability for upgrading facilities to provide available care, especially in rural, underserved areas (WHO et al., 2009, p. 41) . From a human rights accountability standpoint, ethnographic information should be supplemented to the distribution of facilities to discern possible patterns of discrimination in accessibility (UNITED NATIONS, 2000, para. 12) .
In Scenario 2, there are nine functioning EmOC facilities, including some in rural areas, and two of these provide comprehensive care. However, very few women who require EmOC are being cared for in these facilities (met need for EmOC is 8%) (WHO et al., 2009, p. 42) . Low use of EmOC could be attributable to lack of accessibility (whether geographic, economic in the form of user fees or other barriers and/or lack of accessible information) as well as to lack of cultural acceptability, and/or perceived/actual lack of quality. All of these point to failures of accountability. However, they require distinct solutions. In order to discern the nature of the accountability gaps underlying low use, a number of investigative methods might be used by the government or advocacy groups, including community-based surveys, community focus groups, interviews with staff, direct observation of the operation of the facilities and a review of the record-keeping systems (WHO et al., 2009, p. 42) .
In Scenario 3, there are 13 EmOC facilities including three comprehensive ones (which includes blood storage and surgical capacity), and they seem to be well-distributed in terms of rural-urban areas. Fully a quarter of births take place in facilities and met need for EmOC is almost two-thirds. However, the direct obstetric case fatality rate is very high at 15% (with a maximum acceptable level of 1%). In this scenario, the quality of care in the EmOC facilities must be the first concern in terms of identifying accountability gaps (WHO et al., 2009, p. 42) . Furthermore, in this case, maternal death audits and verbal autopsies can prove extremely useful in discerning whether high case fatalities relate to late presentation or to the management of care, provided that they meet the conditions laid out above.
The selection and application of indicators is far from a technical issue; dignity includes access to blood and sutures and we need a way to measure that access if accountability is to be meaningful. By linking the government responsibility for AAAQ, with the evidence we find regarding specific obstacles to women getting the necessary care, we can see that maternal deaths are the foreseeable result of systematic failures with respect to policy, programming and budgeting decisions, in addition to social and cultural factors. Thus, to the extent this information is made publicly available, donors, advocates and governments need no longer discuss abstract accountability for realizing the right to maternal health. Rather, it becomes possible to identify very concrete ways in which ministries of health can operationalize their legal obligations to fulfill the right to maternal health.
It is a substantial positive step toward accountability that Countdown to 2015 now includes an indicator on the availability of EmOC facilities in its global tracking. However, such tracking requires needs assessments and ongoing measurements of EmOC facilities, which have not been done in all countries, including many with high levels of maternal mortality. Although the EmOC indicators have been applied in approximately 50 countries ( WHO et al., 2009) , they have not always been used at the national level or on a continuing basis. A major step toward accountability would be to institute the continuous gathering and use of this data in health systems around the world, including both public and private facilities, and to ensure that the information is widely accessible.
Governments bear the primary responsibility under international law for selecting and using appropriate indicators, as well as for providing the public with transparent access to information regarding their measurement and implications. However, as donors and international agencies often drive the use of indicators, this is an area in which they can play an especially important role, through bilateral health assistance as well as the MDGs process. For its part, the HRC could promote meaningful accountability by having states report on the availability of EmOC facilities, if not all of the EmOC indicators, as part of universal periodic review, and encouraging states that have not done so to adopt the EmOC indicators. UN treaty-monitoring bodies could take similar measures to emphasize the importance of monitoring the use and availability of EmOC in addition to family planning, skilled birth attendance and other areas, in meeting maternal health-related obligations under relevant human rights treaties.
National and district-level initiatives are crucial but the importance of regular monitoring and evaluation, and initiatives taken at the facility-level should not be overlooked to increase transparency, responsiveness and participation in the health system, which are all crucial to a human rights-based approach to accountability (GILL et al., 2005, p. 192). Changes as simple as requiring that prices for any services or medications be posted clearly, and not subject to negotiation, or that staff wear name tags so patients can identify them by name can shift attitudes and relationships between providers and patients markedly. Such reforms are not just important for maternal health, but for all of the health issues addressed within the facility and through its community outreach.
Facility-based accountability initiatives should be implemented in such a way as to be respectful of the staff’s rights, as well as the rights of patients. Not only should health workers not be scapegoated for institutional failures, they should also not be subject to unreasonable demands. For example, no single staff member can be expected to work ‘24/7’ so that there is always coverage; nor can they be expected to dip into their own salaries to pay for medicines or supplies for women experiencing obstetric emergencies. On the contrary, front-line health workers can be encouraged to participate in resolving the accountability-deficits in their facilities by creating incentives for both the reporting and addressing of issues. Personal and institutional leadership has proven instrumental in implementing rights-based approaches to accountability at the facility level (SCOTTISH HUMAN RIGHTS COMMISSION, 2009) .
However, the users of health facilities, whether private or public, also need to be able to file grievances when they face mistreatment, discrimination, or inadequate care (HUMAN RIGHTS WATCH, 2010) . Grievance redressal mechanisms must be accessible to all users and family members, including illiterate persons who cannot file written complaints. Moreover, in order to be effective they must permit addressing systemic issues that go beyond the facility.
Further, community participation in oversight of the facility should go beyond grievance redressal. In Peru, for example, the CLAS (Local Committees for Administration in Health) facilities involve local community members in managing councils that engage in planning, financial auditing and oversight of the facilities, along with the professional staff. Similar schemes exist in other countries, and are sometimes coupled with community-based human rights education. Such schemes should be studied to discern best practices in making facilities accountable to local communities for maternal and other health care, and for enabling local community members, and women in particular, to appropriate their sense of being rights-holders demanding legal and social entitlements (YAMIN et al., 2007) .
The objective is to establish what Lynn Freedman (2003) refers to as “constructive accountability”—a new dynamic of entitlement and obligation. Implemented effectively, facility-based accountability can foster fundamental changes in attitudes among both community members as well as health staff about their rights and responsibilities, and the role of the health system.
Monitoring alone is insufficient to produce human rights-based accountability (POTTS, 2008) . Fundamental to the force of rights is their binding legal nature. Judicial and quasi-judicial remedies therefore have a key role to play in at least four areas related to the right to health, and to maternal, sexual and reproductive health in particular: implementation of existing laws and policies; reform of policies and budgets that fail to take reasonable account of health rights; removal of legal restrictions on care; and challenges to systemic violations of women’s maternal and reproductive health rights in practice.
First, remedies should be available to ensure accountability for the implementation of existing laws and policies. It is unfortunately all too common for legislation and policies relating to reproductive and sexual health not to be implemented through adequate regulations. For example, in the case of Paulina Ramirez v Mexico (IACHR, 2007) , the Center for Reproductive Rights together with the Reproductive Choice Information Group (GIRE, for its Spanish acronym) brought a petition to the IACHR in 2002 involving the failure of the government to enact adequate regulations relating to the access to abortion in rape cases, which was provided for under law ( IACHR, 2007) . The case was settled with the Mexican government through an amicable resolution procedure, whereby the government agreed not only to compensate the named petitioner but also to issue a decree regulating guidelines for access to abortion for rape victims (IACHR, 2007) . Moreover, the process of litigation and the surrounding mobilization on the issue played an important role in changing the public debate around abortion in Mexico and leading to the eventual liberalization of the abortion law in Mexico City.
In March, 2010, the Delhi High Court not only ordered a maternal death audit to be carried out in relation to the death of Shanti Devi, a woman from a scheduled caste who had faced severe discrimination in the health system, but also called for the proper implementation of state-sponsored schemes relating to maternal and child health care for the poor. Citing both international law and prior orders of the Supreme Court, the Delhi Hight Court called for eliminating onerous burdens of proving indigence to access reproductive health services, ensuring the portability of benefit schemes across states and guaranteeing cash assistance to women in need (INDIA, Laxmi Mandal v Deen Dayal Haringer Hospital & Ors Writ Petition , 2010).
Second, remedies can achieve reforms of policies and budgets that do not adequately protect health rights. In the now well-known Treatment Action Campaign case ( SOUTH AFRICA, Minister of Health v. Treatment Action Campaign , 2002) , the South African Constitutional Court found the restriction of Nevirapine treatment for prevention of mother-to-child transmission (PMTCT) to 18 pilot sites to be unreasonable in light of its constitutional obligations relating to the right t o health. The Court not only ordered the extension of PMTCT to the whole country, but also called for a national plan of action with regard to PMTCT and established itself as guardian of the implementation of that plan of action.
The Colombian Constitutional Court has held that reducing the national budget for the subsidized health insurance scheme, which provides coverage to the poor, was inconsistent with the government’s obligations relating to the right to health. The Court considered such budgetary reductions to constitute impermissible retrogression, especially as they would affect the most vulnerable sectors of Colombian society (COLOMBIA, 2000, 2004) .
Third, remedies must be available to challenge legal barriers to care that are discriminatory or directly violate health rights. Abortion restrictions have produced substantial litigation of this type. For example, in a pair of important cases, the Colombian Constitutional Court declared unconstitutional the prohibition of therapeutic abortions as violating women’s rights to health and life with dignity (COLOMBIA, 2006) . The Court later mandated that all health institutions ensure access to providers who would perform such abortions, noting that conscientious objection was a right of individuals and not institutions (COLOMBIA, 2009). Importantly, the Court’s ruling in this case as in others (COLOMBIA, 2008) applies to both private and public providers. Indeed, judicial intervention has been important in setting out the scope of private actors’ obligations with respect to providing care in a number of countries.
After Nicaragua revised its penal code in 2008 to include a total ban on abortion, even when a woman’s life is at risk, a coalition of non-governmental organizations in Nicaragua and around the region brought a case to the IACHR (IACHR, “Amelia”, Nicaragua, 2010) challenging the provisions of the law as violating inter alia the rights to life and health. The IACHR issued precautionary measures in the case, ordering the Nicaraguan government to ensure that the petitioner had access to appropriate medical treatment for her condition. The case has been accompanied by mobilization around the issue, at both the national level and through Amnesty International at the international level (AMNESTY INTERNATIONAL, Nicaragua, 2009a).
Fourth, legal remedies are essential in cases where there are systemic violations of women’s health rights in practice. For example, legal recourse proved a pivotal part of a larger strategy of accountability in Peru when between 1996 and 1998 an estimated 260,000 overwhelmingly indigenous women were sterilized without fully informed consent and under conditions where their rights to health and lives were at risk. A coalition of Peruvian NGOs litigated the emblematic case of Maria Mamérita Mestanza Chávez (IACHR, Peru v. Maria Mamérita Mestanza Chávez, 2000) , in which a woman was involuntarily sterilized and later died as a result of the operation as emblematic of a pattern of violations of fundamental rights and discrimination against indigenous women in Peruvian society. After the case was dismissed in the Peruvian legal system, these NGOs successfully resolved a petition in the Inter-American system.
Similarly, in 2008 the Center for Reproductive Rights brought a petition to the Committee on the Elimination of Discrimination against Women (CEDAW) against Brazil in relation to an emblematic case of systematic de facto discrimination against Afro-descendants in maternal health care in that country (UNITED NATIONS, Alyne da Silva Pimentel v. Brazil , 2007) . In the first maternal mortality case to be brought before CEDAW, the Center, together with Brazilian partner Advocaci, asked for the government not only to compensate the petitioner’s surviving family, but also to prioritize the reduction of maternal mortality in practice, including by training providers, establishing and enforcing protocols, and improving care in vulnerable communities.
In short, the use of remedies in these ways goes far beyond restitution of a pre-existing equilibrium or promises of non-repetition. Rather, judicial and quasi-judicial interventions can play important roles in a larger accountability strategy aimed at transforming discriminatory and exclusionary health systems and practices that bear on women’s maternal and reproductive health and well-being.
In addition to judicial remedies, National Human Rights Institutions (NHRIs) can sometimes promote systemic accountability for the progress of maternal health goals, as well as for violations of maternal health-related rights. Over the past decade in Peru, for example, the Defensoría del Pueblo (Human Rights Ombuds Office) has actively pursued monitoring and oversight of reproductive and maternal health rights. This has led, inter alia , to revised regulations and policies relating to issues ranging from informed consent to regulations regarding traditional birthing positions (PERU, 1999; YAMIN et al., 2007; PERU, 2005) . Unfortunately, Peru is an exception. Given the current interest from donor states and foundations in NHRIs, it would be important to address systematically limitations on budgets, human resources, skill sets and mandates that are currently preventing the majority of NHRIs from being effective accountability mechanisms in the realm of maternal health and other areas (SRIPATI, 2000) .
Many of the decisions that affect the scope of women’s rights to maternal health in the global South are taken by governments in the North and in international organizations controlled by member states from the North. The ESC Rights Committee has been clear: “For the avoidance of any doubt, the Committee wishes to emphasize that it is particularly incumbent on States parties and other actors in a position to assist, to provide ‘international assistance and cooperation, especially economic and technical’ which enable developing countries to fulfill their core and other obligations [including their core obligations relating to maternal and reproductive health]” (UNITED NATIONS, 2000, para. 45).
Nevertheless, the contours of such obligations are not clear and international declarations regarding obligations of international assistance and cooperation remain extraordinarily weak. The Paris Principles on Aid Effectiveness, for example, emphasize “harmonization” and “alignment” without binding commitments based on rights (OECD, 2008) . The Accra Agenda for Action is somewhat stronger than the Paris Principles, calling for assistance to be done “in ways consistent with their agreed international commitments on gender equality, human rights, disability and environmental sustainability.” (OECD, 2008). However, this wording is not followed by the elaboration of specific obligations of support.
Moreover, unlike the other MDGs, MDG 8, which calls for actions from donor countries sets no targets. In general “the global partnership for development” envisioned in MDG 8 has not materialized around maternal and reproductive health, and basic health systems improvements (UNITED NATIONS, 2010b) . Meaningful inclusion of human rights in the MDGs, and into development practice more broadly, demands that targets and corresponding indicators be established through which to hold donor states accountable, as well as national governments in the global South. Those indicators should relate not merely to increasing sustained support for child and maternal health (MDGs 4 and 5, respectively) and health systems more broadly, but also to changes in a wide array of other policies that affect the possibilities of women to enjoy their rights to maternal health.
But such indicators alone are insufficient. Promoting accountability of donor states and international financial institutions requires concerted efforts to raise the costs of non-compliance with both obligations to refrain from policies and actions that undermine the right to health and to provide affirmative economic, as well as technical, assistance ( UNITED NATIONS, 2004b; UNITED NATIONS, 2006a) . Those costs can be financial, political and social. For example, the HIV/AIDS movement has been particularly effective in shifting the cost-benefit calculus of international actors, including donor states and transnational corporations, as well as governments regarding policies and funding relating to access to anti-retrovirals and HIV/AIDS generally. It is still unclear whether increasing engagement by human rights NGOs, including Amnesty International’s important global campaign on maternal mortality, will lead to mobilizing a sustained international movement on maternal health that could exert substantial pressure on donor states. Such pressure would relate to refraining from doing harm, as well as to economic and technical assistance.An obvious example with respect to the obligation to “do no harm”—to refrain from actions that undermine maternal health—relates to the recruitment of health care workers from countries in the global South which are facing dire shortages of health care personnel to meet their right to health obligations. As a policy briefing on MDG 5 from Realizing Rights states: “Donor countries must ensure policy coherence in this respect. Moreover, not addressing health worker migration undermines donor credibility – why build up health systems in developing countries just to take away precious human resources from them? Policy coherence on this is critically important.” (REALIZING RIGHTS, 2010) . In May, 2010, the World Health Assembly unanimously adopted a global Code of Practice on the international recruitment of health personnel (WORLD HEALTH ASSEMBLY, 2010) . The Code calls for voluntary commitments to adopt responsible recruitment policies, but its existence now provides a framework that may encourage cooperation as well as potentially be used to raise the political costs of non-compliance for any individual country that fails to adopt and abide by such commitments.
Second, donor governments must increase economic assistance, as well as technical support. MDG 5 has been the most underfunded MDG and, not surprisingly, has shown very uneven progress (OECD, 2006; FREEDMAN, L.P. et al., 2007, p. 1133; UNITED NATIONS, 2010b) . Although a 2010 Lancet study shows some promising evidence of improvement, it remains clear that enormous increases in global health funding over the last decade have not translated into the necessary investments in basic health services and reproductive health (HOGAN et al., 2010; THE WORLD BANK, 2009; OECD, 2009) . Even the most optimistic picture presents great disparities in progress, and global levels of maternal mortality are far higher than that required to achieve the 75% overall reduction since 1990 levels called for under the MDGs ( HOGAN et al., 2010; HILL et al., 2007, p. 1311; COUNTDOWN TO 2015, 2010, p. 10) .
Although most maternal and newborn care is funded domestically, many poor countries are simply not in a position to provide the necessary services to save women’s lives. For example, in late 2009, donor agreements made possible the establishment of a free care policy for pregnant and lactating women and infants in Sierra Leone, where Amnesty International had documented that user fees posed one of the greatest barriers to access to care (WAKABI, 2010; AMNESTY INTERNATIONAL, Sierra Leone, 2009b).
Overall, however, while the MDGs have coincided with marked increases in global health funding, this has been largely around HIV/AIDS (OECD, 2009) . Whereas from 1990 to 1998 12% of all donor funding (12% of DAC) was allocated to HIV/AIDS and STI control, over the 1999 to 2004 period, this percentage had risen to 25% (24% DAC) in 2007. In contrast, family planning decreased over the same period from 10% to 6% (14% to 6% DAC), and reproductive health care donor funding showed slight dips from 8% to 6% total donors (7% to 6% DAC) (OECD, 2006) . ODA for maternal, newborn and child health accounted for only 31% of all ODA for health in 2007 (COUNTDOWN TO 2015, 2010, p. 36) .
The issue is not cutting up the ODA pie differently; the issue is increasing the pie. A 2009 UN Report concludes: “Without political will and a firm commitment to population, reproductive health, and gender issues, it is unlikely that the goals and targets of the International Conference on Population and Development and the Millennium Summit will be met” (UNITED NATIONS, 2009b, p. 20) .
A number of authors have argued that the consensus on the need to address the global HIV/AIDS pandemic –because in part the financial, political and social costs of not doing so would be too high for countries in the North, as well as those in the South– has been more important in increasing funding than the targets set out in MDG 6 ( CROSSETTE, 2005, p. 77; HULME, 2009, p. 24) . Moreover, the creation of the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) and the United States President’s Emergency Plan for AIDS Relief created important institutional mechanisms through which to establish donor state commitments. The March 2010 UN Secretary General’s Report on the MDGs states that, in light of the need to improve the quality, predictability and durability of aid, in addition to the quantity, “Pooling of donor resources into multi-donor funds has proved time and again to be a fruitful approach, with great successes, for example, in the control of several infectious diseases” (UNITED NATIONS, 2010b, para. 85) .
In this regard, a number of authors argue that the Global Fund’s mandate might be expanded to include maternal and child health, or health systems broadly (THE LANCET EDITORIAL BOARD, 2010; STARRS; SANKORE, 2010; STARRS, 2009; CORNETTO et al., 2009) . Such proposals go significantly beyond integrating maternal and reproductive health into HIV/AIDS programs, which is feasible under the current mandate.
The Global Fund, which was established in 2002, is far from a perfect mechanism. Criticisms regarding sustainability, inefficiency and lack of transparency have plagued it, resources have not been allocated equitably among HIV/AIDS, tuberculosis and malaria, and interventions have at times undermined rather than strengthened health systems (HALL, 2005) . Moreover, the creation of a mechanism cannot stand alone; constant pressure from the HIV/AIDS movement in different countries has played an important role in sustaining financial commitments to the Global Fund.
Nevertheless, expansion and adaptation of the Global Fund presents the possibility of engaging donor states in long-term commitments to maternal health and health systems more broadly. The framework established through the Global Fund critically does not assume that addressing critical health needs be done in a “sustainable” way— i.e ., that aid is for a time certain and efforts should be directed at making poor governments fend for themselves despite a lack of financial, material and human resources and a global architecture that stacks the odds against them ( CORNETTO et al., 2009; THE GLOBAL FUND, 2007) . Instead, there is an assumption of some international responsibility and a concomitant ongoing international commitment for funding activities to address HIV, TB and malaria (UNITED NATIONS, 2006a, para. 41) . There desperately needs to be a similar global commitment for investing in health systems, and maternal health in particular. Expanding and adapting the Global Fund, or creating a similar mechanism, would demonstrate serious donor commitment as well as potentially raise the political and social costs of erratic suspensions of aid for health systems in the long term.
Maternal mortality is not principally a medical problem; it is primarily a social problem and a problem of political will at both the national and international level. The reason that hundreds of thousands of women and girls are still dying every year is not because we do not know how to save them. Women are still dying in massive numbers around the world because women’s lives are not valued, because their voices are not listened to, because they are discriminated against and excluded in their homes and communities—and by health care systems that do not prioritize their needs.
I have argued here that promoting transformative accountability with respect to fulfilling the right to maternal health requires more than decrying the scandalous injustice of those deaths, and more than demanding that states act consistently with their international legal obligations. It requires translating the powerful normative discourse of human rights into operational guidance and concrete tools for development practitioners, health planners and service providers, as well as the users of health systems. Transformations of health systems are unlikely to occur with punitive approaches that lead to, intentionally or otherwise, a focus on individual sanctions. They are far more likely to occur by putting into place measures that promote systemic and institutional changes, which in turn foster different relations between providers and users of health services.
National governments should be held accountable for decisions from the initial situation analysis and design of plan of action regarding maternal health to budgeting, monitoring and evaluation, and the provision of remedies. At every stage, transparency, access to information and meaningful public participation are crucial to rights-based accountability. Additionally, donor governments need to be held responsible for policy coherence and increased financial assistance for health systems and maternal health, which will require innovating mechanisms as well as political and social mobilization to raise the economic, political and social costs of non-compliance.
Further, there is an important relationship between international bodies and mechanisms and national ones in terms of promoting accountability. UN treaty-monitoring bodies and special procedures, together with the Human Rights Council and other regional bodies such as the IACHR and the African Commission, have key roles to play in ensuring that laws and policies are consistent with governments’ human rights obligations, that adequate progress is being made consistent with appropriate indicators on a non-discriminatory basis; that sufficient resources are being allocated effectively; that efforts to reduce maternal mortality give special attention to marginalized populations; and that adequate mechanisms of redress exist at the national level.
A human rights approach to MMM calls for subverting a wide range of the “pathologies of power” that systematically marginalize women and their health needs (FARMER, 2005) . However, challenging the power structures that prevent women from having choices over their lives must include those in the health system that condemn women to needless suffering and death. As Paul Hunt and Gunilla Backman write: “In any society, an effective health system is a core institution, no less than a fair justice system or democratic political system. … It is only through building and strengthening health systems that it will be possible to secure sustainable development, poverty reduction, economic prosperity, improved health for individuals and populations, as well as the right to the highest attainable standard of health” (HUNT; BACKMAN, 2008) . Improving health systems cannot be seen as a technocratic exercise; by bringing human rights to bear, transforming health systems can and should be understood as a means of constructing social citizenship for women in a society—and most critically for poor, rural and marginalized women (FREEDMAN, 2005) . In a world where women’s reproduction is so heavily cathected, so intimately bound up with religious and cultural power, it is radical indeed to demand that health systems take women’s suffering– and rights– seriously (YAMIN, 2008) .
1. The title of this article echoes that of the MDG Task Force Report on Child and Maternal Health: Who’s got the power?: transforming health systems for women and children. I have benefited from the thinking of so many colleagues in relation to this piece that it would be impossible to acknowledge them all. I am especially grateful to Paul Hunt and Lynn Freedman for their insights about operationalizing human rights approaches in the context of maternal health; to Siri Gloppen, whose ideas regarding the utility of different forms of litigation are very much reflected here; and to Deborah Maine, who has shown me what kinds of programming really make a difference to the millions of women around the world who risk dying in pregnancy and childbirth. All views expressed are personal and do not necessarily reflect those of Amnesty International or the International Initiative on Maternal Mortality and Human Rights.
2. Maternal death is defined as “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes.” For every woman who dies from obstetric complications, approximately 30 more suffer from debilitating morbidities which include conditions such as uterine prolapse and obstetric fistulae. http://www.unfpa.org/mothers/morbidity.htm.
3. ‘The obligation to respect requires States to refrain from interfering directly or indirectly with the enjoyment of the right to health. The obligation to protect requires States to take measures that prevent third parties from interfering with article 12 guarantees. Finally, the obligation to fulfil requires States to adopt appropriate legislative, administrative, budgetary, judicial, promotional and other measures towards the full realization of the right to health.’ (UNITED NATIONS, 2000, para. 33).
Bibliography and Other Sources
AMNESTY INTERNATIONAL. 2009a. Nicaragua: Report 2009. Available at: <http://www.amnesty.org/en/region/nicaragua/report-2009>. Last accessed on: 2 Apr. 2010.
______. 2009b. Out of Reach: The Cost of Maternal Health in Sierra Leone. New York. Available at: <http://www.amnesty.org.au/images/uploads/svaw/2566_SierraL_Covreport_web.pdf>. Last accessed on: 27 Mar. 2010.
______. 2010. The State of the World’s Human Rights. Index: POL 10/001/2010.
CENTER FOR REPRODUCTIVE RIGHTS (CRR). 2009. Broken Promises: Human Rights, Accountability and Maternal Death in Nigeria. New York. Available at: <http://www2.ohchr.org/english/bodies/cedaw/docs/ngos/CRR_Nigeria41.pdf>. Last accessed on: 27 Mar. 2010.
CESR. 2009. Rights or Privileges? Fiscal Commitment to the Right to Health, Education and Food in Guatemala: Executive Summary. Madrid. Available at: <http://www.cesr.org/downloads/Rights%20or%20Privileges%20Executive%20Summary%20final.pdf>. Last accessed on: 27 Mar. 2010.
CORNETTO, G. et al. 2009. A global fund for the health MDGs? The Lancet, v. 373, p. 1500-1503.
COUNTDOWN TO 2015. 2008. Statement of Commitment Concerning Maternal, Newborn and Child Survival. Cape Town. Available at: <http://www.countdown2015mnch.org/documents/statementofcommitment_english.pdf>. Last accessed on: 27 Mar. 2010.
______. 2010. 2010 Countdown to 2015 Decade Report (2000-2010). Available at: <http://www.countdown2015mnch.org/reports-publications/2010-report>. Last accessed on: 27 Mar. 2010.
CROSSETTE, B. 2005. Reproductive health and the Millennium Development Goals: the missing link. Family Planning, v. 36, n. 1, p. 71-79.
DANIELS, N. 2008. Just Health: Meeting Health Needs Fairly. New York: Cambridge University Press.
DEFEYTER, K. 2001. World Development Law: Sharing Responsibility for Development. Antwerp: Intersentia.
DEPARTMENT FOR INTERNATIONAL DEVELOPMENT. 2005. How to Reduce Maternal Deaths: Rights and Responsibilities. UK.
GRUSKIN, S.; DANIELS, N. 2008. Justice and human rights: priority setting and fair deliberative process. American Journal of Public Health, v. 98, n. 9, p. 1573-1577.
FARMER, P. 2005. Pathologies of Power: Health, Human Rights, and the New War on the Poor. Berkeley: University of California Press.
______. 2008. Challenging orthodoxies: The road ahead for health and human rights. Health and Human Rights, v. 10, n. 1, p. 6.
FREEDMAN, L.P. 2002. Shifting visions: Delegation policies and the building of a rights-based approach to maternal mortality. Journal of the American Womens Association, v. 57, n. 3, p. 154-158.
______. 2003. Human rights, constructive accountability and maternal mortality in the Dominican Republic: a commentary. International Journal of Gynecology and Obstetrics, v. 82, p. 111-114.
______. 2005. Achieving the MDGs: Health Systems as Core Social Institutions. Development, v. 48, p. 19-24.
FREEDMAN, L.P. et al. 2005. Who’s got the power?: transforming health systems for women and children. London: Earthscan, 185 p.
______. 2007. Practical lessons from global safe motherhood initiatives: time for a new focus on implementation. The Lancet, v. 370, n. 9595, p. 1383-1391.
GILL, Z. et al. 2005. A tool for assessing ‘readiness’ in emergency obstetric care: The room-by-room ‘walk-through’. International Journal of Gynecology and Obstetrics, v. 89, p. 191-199.
THE GLOBAL FUND. 2002. The Framework Document of the Global Fund to Fight AIDS, Tuberculosis and Malaria. Geneva. Available at: <http://www.theglobalfund.org/documents/TGF_Framework.pdf>. Last accessed on: 2 Apr. 2010.
______. 2007. Proposal Form – Round 7. Available at: <http://www.theglobalfund.org/documents/rounds/7/R7_Proposal_Form_en.doc>. Last accessed on: 2 Apr. 2010.
GEORGE, A. et al. 2010. Making rights more relevant for health professionals. Lancet, v. 375, p. 1764-1765.
HALL, J. 2005. The Global Fund for AIDS, tuberculosis, and malaria. StudentBMJ, v. 13, p. 441-484.
HILL, K. et al. 2007. Estimates of maternal mortality worldwide between 1990 and 2005: an assessment of available data. Lancet, v. 370, n. 9595, p. 1311-1319.
HOGAN, M. et al. 2010. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet, v. 375, p. 1609-1623.
HULME, D. 2009. The Millennium Development Goals (MDGs): A short history of the world’s biggest promise. BWPI Working Paper 100. Manchester. Available at: <http://www.bwpi.manchester.ac.uk/resources/Working-Papers/bwpiwp-10009.pdf>. Last accessed on: 27 Mar. 2010.
HUMAN RIGHTS WATCH. 2009. No Tally of the Anguish: Accountability in Maternal Health Care in India. New York. Available at: <http://www.hrw.org/en/reports/2009/10/08/no-tally-anguish-0>. Last accessed on: 27 Mar. 2010.
______. 2010. Unaccountable: Addressing Reproductive Health Care Gaps. New York.
HUNT, P. 2008. Maternal Health and Human Rights. Lancet, v. 371, n. 9608, p. 203.
HUNT, P.; BACKMAN, G. 2008. Health systems and the right to the highest attainable standard of health. Health and Human Rights, v. 10, n. 1, p. 81-92.
INTERNATIONAL CONFERENCE ON POPULATION AND DEVELOPMENT (ICPD). 1994. Programme of Action of the United Nations International Conference on Population and Development. Cairo. Available at: <http://www.dirittiumani.donne.aidos.it/>. Last accessed on: 2 Apr. 2010.
INTERNATIONAL INITIATIVE ON MATERNAL MORTALITY AND HUMAN RIGHTS (IIMMHR). 2010. About Maternal Mortality. New York. Available at: <http://righttomaternalhealth.org/about-maternal-mortality>. Last accessed on: 27 Mar. 2010.
INTERNATIONAL BUDGET PARTNERSHIP. 2001. A Guide to Budget Work for NGOs. Washington, D.C. Available at: <http://www.internationalbudget.org/files/guide_to_budget_work.pdf>. Last accessed on: 2 Apr. 2010.
______. 2010. 6 Question Campaign. Request Protocol. Available at: <http://www.internationalbudget.org/pdf/6QC_Protocol_English.pdf>. Last accessed on: 2 Apr. 2010.
KEITH-BROWN, K. 2005 Investing for Life: Making the Link between Public Spending and the Reduction of Maternal Mortality. Mexico City: Fundar, Centro de Análisis e Investigación.
KGAMPHE, L.; MAHONY, L. (Ed.). 2004. Using Government Budgets as a Monitoring Tool: The Children’s Budget Unit in South Africa. Minneapolis. Available at: <http://www.newtactics.org/sites/newtactics.org/files/Kgamphe_Budgets_update2007.pdf>. Last accessed on: 2 Apr. 2010.
KRAFCHIK, W. 2010. 6 Question Campaign. New Tactics in Human Rights, 1 Mar. Available at: <http://www.newtactics.org/en/blog/new-tactics/using-budgets-monitoring>. Last accessed on: 2 Apr. 2010.
THE LANCET EDITORIAL BOARD. 2010. The Global Fund: replenishment and redefinition in 2010. Lancet, v. 375, n. 9718, p. 865.
LANGFORD, M. 2008. Claiming the Millennium Development Goals: A Human Rights Approach. New York: United Nations.
LONDON, L. 2008. What is a Human-Rights Based Approach to Health and Does it Matter? Health and Human Rights, v. 10, p. 63-77.
MAINE, D. 1999. What’s so special about maternal mortality? Safe Motherhood Initiatives: Critical Issues. London: Blackwell, p. 175-182.
MCKAY, B. 2010. White House Proposes 9% Increase in Global-Health Funding. Wall Street Journal, Feb.
NIGERIA. 2009. National Population Commission. Standard DHS, 2008. Calverton, MD: ICF Macro.
ORGANIZATION FOR ECONOMIC CO-OPERATION AND DEVELOPMENT (OECD). 2006. Recent Trends in Official Development Assistance to Health. Paris. Available at: <http://www.oecd.org/dataoecd/1/11/37461859.pdf>. Last accessed on: 27 Mar. 2010.
______. 2008. Paris Declaration on Aid Effectiveness and Accra Agenda for Action. Paris. Available at: <http://www.oecd.org/dataoecd/11/41/34428351.pdf>. Last accessed on: 27 Mar. 2010.
______. 2009. Measuring Aid to Health. Paris. Available at: <http://www.oecd.org/dataoecd/44/35/44070071.pdf>. Last accessed on: 27 Mar. 2010.
PERU. 1999. Defensoria del Pueblo. Informe Defensorial No. 27: La aplicación de la anticoncepción quirúrgica y los derechos reproductivos II. Lima. Available at: <http://www.defensoria.gob.pe/inform-defensoriales.php>. Last accessed on: 27 Mar. 2010.
______. 2005. Defensoria del Pueblo. Informe Defensorial No. 90: Supervisión a los Servicios de Planificación Familiar IV. Lima. Available at: <http://www.defensoria.gob.pe/inform-defensoriales.php>. Last accessed on: 27 Mar. 2010.
POTTS, H. 2008. Accountability and the right to the highest attainable standard of health. Human Rights Centre, University of Essex. Available at: <http://www.essex.ac.uk/human_rights_centre/research/rth/docs/HRC_Accountability_Mar08.pdf>. Last accessed on; 27 Mar. 2010.
PROMSEX. 2010. Demandan a Estado Peruano por AOE. La Republica, Lima, 15 Jan. Available at: <http://promsex.org/articulos/demandan-a-estado-peruano-por-aoe.html>. Last accessed on: 2 Apr. 2010.
REALIZING RIGHTS: THE ETHICAL GLOBALIZATION INITIATIVE. 2010. Briefing Note. Messages on MDG 5 – Maternal Health and Reducing Maternal Mortality.
ROBINSON, M. 2005. What rights can add to good development practice. In: ALSTON, P.; ROBINSON, M. (Org.). Human Rights and Development: Towards Mutual Reinforcement. New York: Oxford University Press, p. 25-44.
ROSENFIELD, A.; MAINE, D.; FREEDMAN, L.P. 2006. Meeting MDG-5: an impossible dream? Lancet, v. 368, n. 9542, p. 1133-1135.
ROTH, K. 2004. Defending Economic, Social and Cultural Rights: Practical Issues Faced by an International Human Rights Organization. Human Rights Quarterly, v. 26, p. 63-73.
SIERRA LEONE. 2009. Statistics Sierra Leone, Ministry of Health and Sanitation Freetown, Sierra Leone. Sierra Leone: Standard DHS, 2008. Calverton, MD: ICF Macro. Available at: <http://www.measuredhs.com/pubs/pub_details.cfm?ID=978&ctry_id=208&SrchTp=>. Last accessed on: 20 May 2010.
SCOTTISH HUMAN RIGHTS COMMISSION. 2009. Human Rights in a Health Care Setting: Making it Work for Everyone: an evaluation of a human rights-based approach at The State Hospital. Glasgow. Available at: <http://www.tsh.scot.nhs.uk/PFPI/docs/Human%20Rights%20-%20Summary%20-%20Dec%202009.pdf>. Last accessed on: 27 Mar. 2010.
SRIPATI, V. 2000. India’s National Human Rights Commission: a shackled commission? Boston University International Law Journal, v. 18, p. 3-46.
STARRS, A. 2009. Funding the Health MDGs. Family Care International, 11 May. Available at: <http://www.familycareintl.org/en/about/27#Funding>. Last accessed on: 2 Apr. 2010.
______; SANKORE, R. 2010. Momentum, mandates and money: achieving health MDGs. Lancet, v. 375, n. 9730, p. 1946-1947.
UNDURRAGA, V.; COOK, R. 2009. Constitutional incorporation of international and comparative human rights law: the Colombian Constitutional Court Decision C-355/2006. In: WILLIAMS, S.H. (Org.). Constituting Equality: Gender Equality and Comparative Constitutional Law. Cambridge: Cambridge University Press, p. 215-247.
UNITED NATIONS. 1966. International Covenant on Economic, Social and Cultural Rights, UN Doc. GA Res 2200A (XXI) 16 Dec. 1966. Available at: <http://www2.ohchr.org/english/law/cescr.htm>. Last accessed on: 20 May 2010.
______. 1998. Development Programme. Integrating Human Rights with Sustainable Human Development. New York. Available at: < http://hurilink.org/tools/UNDP_integrating_hr.pdf. Last accessed on: 27 Mar. 2010.
______. 1999. Committee on the Elimination of Discrimination against Women (CEDAW). General Recommendation No. 24: Women and Health. 20th session. Available at: <http://www.un.org/womenwatch/daw/cedaw/recommendations/recomm.htm#recom24>. Last accessed on: 7 Apr. 2010.
______. 2000. Committee on Economic, Social and Cultural Rights (CESCR). General Comment 14 on the Right to Health, UN Doc. E/C.12/2000/4. Available at <http://www.unhchr.ch/tbs/doc.nsf/(symbol)/E.C.12.2000.4.En>. Last accessed on: 20 May 2010.
______. 2004a. Development Group. Hacia el cumplimiento de los objetivos de desarrollo del milenio en el Perú. Geneva. Available at: <http://www.undg.org/archive_docs/5504-Peru_MDG_Report_-_MDGR.pdf>. Last accessed on: 27 Mar. 2010.
______. 2004b. Commission on Human Rights. Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Paul Hunt, UN Doc. E/CN.4/2004/49, para. 45, 60th Session. Available at: <http://www.unhchr.ch/Huridocda/Huridoca.nsf/(Symbol)/E.CN.4.2004.49.En.>. Last accessed on: 20 May 2010.
______. 2005. Millennium Project. Who’s Got the Power? Transforming Health Systems for Women and Children. New York. Available at: <http://www.reliefweb.int/rw/rwb.nsf/db900SID/MYAI-83M3CB?OpenDocument>. Last accessed on: 2 Apr. 2010.
______. 2006a. Political Declaration on HIV/AIDS, UN Doc. A/RES/60/262, 60th Session. Available at: <http://data.unaids.org/pub/Report/2006/20060615_hlm_politicaldeclaration_ares60262_en.pdf>. Last accessed on: 2 Apr. 2010.
______. 2006b. Special Rapporteur on the Right to Health. Report of the UN Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health to the UNGA, UN Doc. A/61/338, 61st Session. Available at: <http://daccess-dds-ny.un.org/doc/UNDOC/GEN/N06/519/97/PDF/N0651997.pdf?OpenElement>. Last accessed on: 20 May 2010.
______. 2009a. Human Rights Council. Resolution 11/8. Preventable maternal mortality and morbidity and human rights, UN Doc. A/HRC/RES/11/8, 11th Session. Available at: <http://ap.ohchr.org/documents/E/CDH/resolutions/A_CDH_RES_11_8.pdf>. Last accessed on: 27 Mar. 2010.
______. 2009b. Commission on Population and Development. Flow of financial resources for assisting in the implementation of the Programme of Action of the International Conference on Population and Development: Report of the Secretary-General, UN Doc. E/CN.9/2009/5, 42th Session. Available at: <http://daccess-dds-ny.un.org/doc/UNDOC/GEN/N09/215/67/PDF/N0921567.pdf?OpenElement>. Last accessed on: 27 Mar. 2010.
______. 2010a. Office of the High Commissioner for Human Rights (UN OHCHR). Report of the Office of the United Nations High Commissioner for Human Rights on preventable maternal mortality and morbidity and human rights, UN Doc. A/HRC/14/39. (Advance Edited Version). Available at: <http://www2.ohchr.org/english/bodies/CDHouncil/docs/14session/A.CDH.14.39_AEV-2.pdf>. Last accessed on: 20 May 2010.
______. 2010b. Keeping the promise: a forward-looking review to promote an agreed action agenda to achieve the Millennium Development Goals by 2015. Report of the Secretary-General, UN Doc. A/64/665, 64th Session. Available at: <http://www.reliefweb.int/rw/RWFiles2010.nsf/FilesByRWDocUnidFilename/MYAI-83M3CBfull_report.pdf/$File/full_report.pdf>. Last accessed on: 2 Apr. 2010.
UVIN, P. 2004. Human Rights and Development. Bloomfield, CT: Kumarian Press.
WAKABI, W. 2010. Mothers and infants to get free health care in Sierra Leone. Lancet, v. 375, n. 9718, p. 882.Original Text).
THE WORLD BANK. 2009. World’s progress on maternal health and family planning is insufficient. News and Broadcast, 9 Jul. Available at: <http://web.worldbank.org/WBSITE/EXTERNAL/NEWS/0,,contentMDK:22241448~pagePK:64257043~piPK:437376~theSitePK:4607,00.html>. Last accessed on: 27 Mar. 2010.
WORLD HEALTH ASSEMBLY. 2006. International migration of health personnel: a challenge for health systems in developing countries. A59/18, 59th Session. 4 May 2006. Available at: <http://apps.OMS.int/gb/ebwha/pdf_files/WHA59/A59_18-en.pdf>. Last accessed on: 2 Apr. 2010.
______. 2010. WHO Code of practice on the international recruitment of health personnel. Available at <http://www.who.int/hrh/migration/code/full_text/en/index.html>. Last accessed on: 2 Apr. 2010.
WORLD HEALTH ORGANIZATION (WHO). 2004. Beyond the Numbers: Reviewing Maternal Deaths and Complications to Make Pregnancy Safer. Geneva. Available at: <http://www.ino.searo.OMS.int/LinkFiles/Reproductive_health_Beyond_the_numbers.pdf>. Last accessed on: 2 Apr. 2010.
WORLD HEALTH ORGANIZATION (WHO) et al. 2009. Monitoring Emergency Obstetric Care: A Handbook. Geneva. Available at: <http://www.unfpa.org/webdav/site/global/shared/documents/publications/2009/obstetric_monitoring.pdf>. Last accessed on: 27 Mar. 2010.
YAMIN, A.E. 2008. Will we take suffering seriously; reflections on what applying a rights framework to health means and why we should care. Health and Human Rights, v. 10, n. 1, p. 45-63.
YAMIN, A.E. et al. 2007. Deadly Delays: Maternal Mortality in Peru – A Rights-Based Approach to Safe Motherhood. Cambridge: Physicians for Human Rights. Available at: <http://physiciansforhumanrights.org/library/documents/reports/maternal-mortality-in-peru.pdf>. Last accessed on: 27 Mar. 2010.
YAMIN, A.E.; MAINE, D. 1999. Maternal mortality as a human rights issue: measuring compliance with international treaty obligations. Human Rights Quarterly, v. 21, n. 3, p. 563-607.
Jurisprudence
ARGENTINA. 1998. Poder Judicial de la Nación. Case No. 31.777/96. Viceconte, Mariela Cecilia. v. Argentinian Ministry of Health and Social Welfare, Decision of June 2.
COLOMBIA. 2000. Constitutional Court. Judgment C-1165, Sentence.
______. 2004. Constitutional Court. Judgment C-040, Sentence.
______. 2006. Constitutional Court. Judgment C-355, Sentence.
______. 2007. Constitutional Court. Judgment C-521, Sentence.
______. 2008. Constitutional Court. Judgment T-760, Sentence.
______. 2009. Constitutional Court. Judgment T-388, Sentence.
INDIA. 2010. High Court of Delhi. Laxmi Mandal v Deen Dayal Haringer Hospital & Ors Writ Petition, Sentence.
INTER-AMERICAN COMMISSION ON HUMAN RIGHTS (IACHR). 2000. Case 12.191 Peru v. Maria Mamérita Mestanza Chávez, Report No. 66/00. Sentence, 3 October.
______. 2007. Case 161.02. Paulina del Carmen Ramirez Jacinto v Mexico, Report No. 21/07, Friendly Settlement, 9 March.
______. 2010. Case PM 43-10. “Amelia”, Nicaragua, Sentence, 26 February.
SOUTH AFRICA. 2002. Constitutional Court. Case (5) SA 721 (CC). Minister of Health v. Treatment Action Campaign, Sentence, 5 July.
UNITED NATIONS. 2007. Committee on the Elimination of Discrimination against Women (CEDAW). Alyne da Silva Pimentel v. Brazil, UN Doc. CEDAW/C/BRA/CO/6.